|
Blog Author: Kearston Wishnefsky, Intern Counselor Soon we'll be observing the end of Daylight Savings Time on Sunday 11/6/22, by changing our clocks an hour forward as we approach the beginning of Winter. The time change means adjusting to earlier nightfall, preparing for colder weather, and planning for more indoor activities. But for some, the changing time and seasons brings unexpected changes in our feelings and behaviors.
Seasonal Affective Disorder (SAD), often referred to as seasonal depression, is a form of depression that comes and goes with the changing of the seasons. Although symptoms of SAD are more commonly associated with Fall/Winter as the weather gets cooler and the days get shorter, it's not uncommon for people to experience symptoms at the end of Winter as Spring approaches as well. So, what does SAD look like? In essence, SAD is a series of symptoms typically associated with depression, but symptoms occur only for a short period of time, at about the same time each year during seasonal changes. Commonly reported symptoms of SAD may include irritability/agitation, changes in appetite or sleep patterns, loss of energy or motivation, difficulty concentrating or making decisions, decreased sex drive, feelings of hopelessness or worthlessness, and loss of interest in activities or socializing. How might these symptoms differ if SAD occurs during the Fall/Winter as opposed to the Spring/Summer? In the colder months, people with SAD often sleep more and eat more, and as a result gain weight. In contrast, SAD symptoms in the warmer months often include insomnia, reduced appetite with associated weight loss, as well as some symptoms of anxiety. There are a few things you can do to be proactive against SAD: - Spend at least 30 minutes a day outside in the fresh air before the sun sets—bonus points if you use that time to get some physical exercise in! - Turn off tech at least 2 hours before bed—instead, choose an activity that doesn’t involve unnatural bright light, such as reading, a jigsaw puzzle, playing cards, or a board game - Keep to a consistent bedtime and wake-up routine - Eat a well-balanced diet and drink plenty of water - Keep in touch with your loved ones regularly for social connection If you still find yourself experiencing symptoms related to SAD, don’t hesitate to seek support. Reach out to your therapist for help. If you don’t have a therapist, your primary doctor can provide you with referrals, or you can search online for local mental health providers in your area. If you have an insurance plan, call the customer service number on the back of your insurance card, and ask for a list of available providers. As with any depressive disorder, more severe symptoms may include suicidal thoughts. If you’re experiencing suicidal thoughts, you can access immediate support by contacting the Suicide & Crisis Lifeline: Dial or message 988 to talk or text, or go to https://988lifeline.org/ to chat live with someone who can help.
0 Comments
Blog Author: Amy Hamby, Intern Counselor Most patients see their therapist weekly and often biweekly. There are many exercises patients can do in between sessions that can assist in future sessions. Occasionally therapist will give their patients “homework” such as journaling and breathing exercises. Depending on what someone is looking to get out of therapy there is plenty of outside work someone can do in between therapy sessions. Below are suggestions.
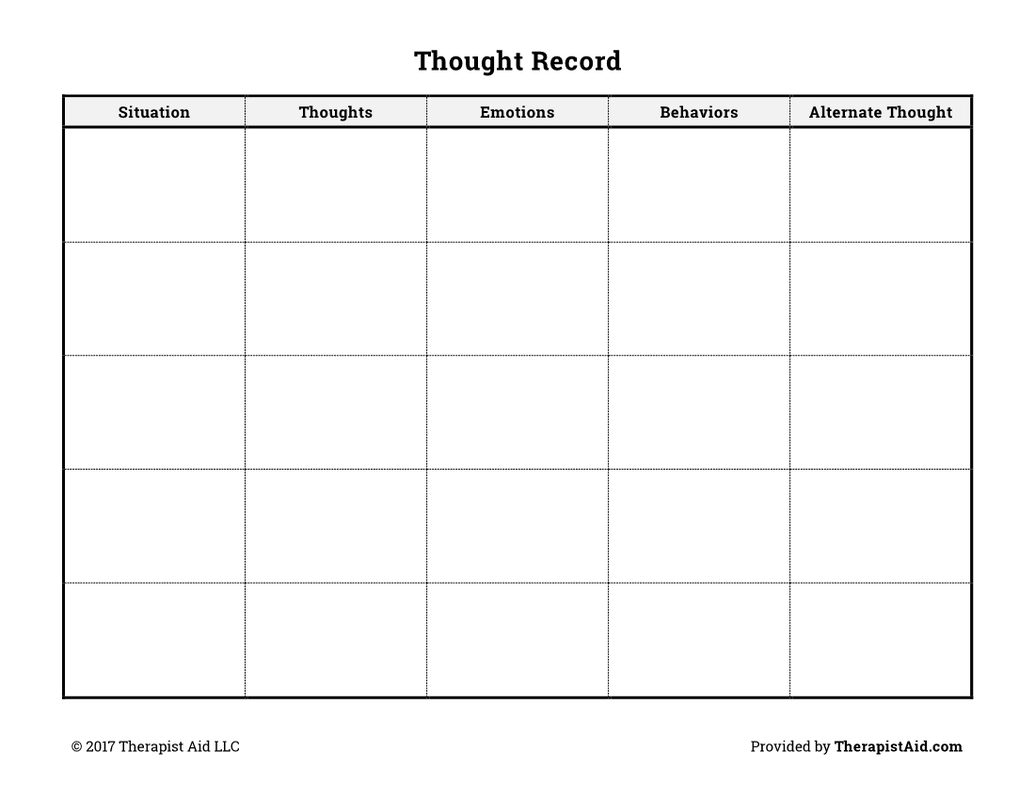
◦ Journaling. You can journal about your thoughts about the session you previously had, some questions you might have for your next session. It’s also a great idea to journal your feelings and thoughts throughout your daily life. Journaling is a great exercise that could be utilized in therapy because often patients forget about certain things and writing allows certain memories to come to the surface. ◦ Meditate. Meditation is a great grounding technique Allowing patients to become more mindful and present. Meditation can start off in smaller increments (1-5 minutes) and increase overtime. ◦ Connecting with nature. This can be done by gardening, combining a meditation outside, walking or doing any type of exercise outdoors. ◦ Going for a walk. Walking is a wonderful, low impact exercise that can assist in relieving stress and anxiety. Going for a walk is also connecting with nature. ◦ Focus on one thing at a time. Making list and prioritizing what needs to get done can help you focus on one task at a time. Often people feel many different emotions after being with their therapist. Many of these exercises can help with the emotions in between sessions along with grounding and becoming more mindful. Blog Author: Amy Hamby, Intern Counselor Cognitive Behavior Therapy (CBT) focuses on recognizing and altering automatic thoughts because these cognitions strongly influence emotions and behavior. (Wright et al., 2017, pg. 125) In other words, CBT is a practical treatment approach that helps clients acquaint themselves with negative thoughts and behaviors, which allows them to view these experiences and change how they reason and respond. Furthermore, it is vital to determine the difference in how thoughts reflect upon how we feel and act and how to respond efficiently throughout the thought process emotionally. Also, your thoughts are what is reoccurring in your outlook, what causes the feelings to occur, and assist with making sense of whatever is happening. Meanwhile, your emotions are how you feel within the moment that makes up the emotional experience Additionally, understanding how to separate one's thoughts and emotions will help the individual with the association of understanding that their thoughts and emotions can influence an emotional response. Individual thoughts make you cognizant of negative thinking and know how to respond effectively. This includes the importance of a thought record, which provides for "features such as labeling cognitive errors, examining the evidence, and generating rational alternatives is usually delayed until the patient gains experience and confidence in identifying automatic thoughts." (Wright et al., 2017, pg. 99) On the other hand, "Emotion is the royal road to cognition because thought patterns linked to significant emotional expression offer rich opportunities for drawing out some of the patient's most important automatic thoughts and schemas." (Wright et al., 2017, pg. 95) Overall, thoughts and emotions can help clients recognize and explore all the different reactions and thoughts that contribute to an individual's actions and how a therapist can assist with ruling out negative emotions, exploring automatic thoughts, and giving the alternative client perspectives on how an individual feels. Below is an example of a thought record.
Thought record - therapist aid. (n.d.). Retrieved August 29, 2022, from https://www.therapistaid.com/worksheets/thought-record Wright, J. H., Brown, G. K., Thase, M. E., & Basco, M. R. (2017). (2nd edition) Learning cognitive-behavior therapy: An illustrated guide. American Psychiatric Publishing, Inc |
Archives
March 2024
|